“HRCT Temporal Bone is a special CT scan that provides detailed images of the ear’s tiny bones and structures—here’s why it’s done.”
High-resolution CT (HRCT) temporal bone imaging reveals intricate ear structures that standard CT scans simply can’t capture. This comprehensive guide serves radiologists, ENT specialists, and radiology residents who want to master temporal bone anatomy interpretation and improve their diagnostic accuracy.
HRCT temporal bone scans provide unmatched detail of the ear’s complex anatomy, from the tiny ossicles in the middle ear to the delicate labyrinthine structures of the inner ear. Understanding these anatomical landmarks is essential for identifying pathology and guiding treatment decisions.
We’ll explore the external and middle ear structures you’ll encounter on every HRCT ear anatomy study, including the tympanic membrane, ossicular chain, and mastoid air cells. You’ll also learn to recognize the intricate inner ear complex anatomy, including the cochlea, semicircular canals, and internal auditory canal. Finally, we’ll cover common pathological findings and how to apply clinical interpretation guidelines that will enhance your temporal bone radiology skills.
Understanding HRCT Technology for Temporal Bone Imaging

High-resolution CT capabilities and advantages over standard CT
High-resolution CT (HRCT) represents a significant leap forward in temporal bone imaging, offering unparalleled detail of the intricate structures within the ear. Unlike standard CT scans, HRCT temporal bone studies use ultra-thin slice thickness, typically ranging from 0.5 to 1.0 millimeters, compared to the 5-10 millimeter slices common in routine body CT imaging. This dramatic reduction in slice thickness allows radiologists to visualize minute anatomical structures that would otherwise be lost in volume averaging.
The superior spatial resolution of HRCT temporal bone imaging reaches approximately 0.1 to 0.2 millimeters, making it possible to clearly distinguish individual ossicles within the middle ear cavity. The malleus, incus, and stapes become distinctly visible, along with their articulations and surrounding soft tissue relationships. Standard CT simply cannot achieve this level of detail due to its inherent technical limitations.
Bone algorithm reconstruction plays a crucial role in HRCT ear anatomy visualization. This specialized reconstruction technique enhances the contrast between different density structures, making the delicate bony labyrinth of the inner ear clearly visible against surrounding soft tissues. The cochlear turns, semicircular canals, and vestibule appear with remarkable clarity, allowing for precise assessment of both normal anatomy and pathological changes.
The high contrast resolution of HRCT also excels at detecting subtle density differences within temporal bone structures. This capability proves invaluable when evaluating conditions like otosclerosis, where small areas of abnormal bone density around the oval window can significantly impact hearing function.
Optimal scanning parameters for temporal bone visualization
Achieving optimal HRCT temporal bone results requires careful attention to multiple technical parameters that work together to maximize image quality while minimizing patient radiation exposure. Slice thickness remains the most critical parameter, with 0.5mm slices providing the gold standard for temporal bone diagnostic imaging. Some protocols use 0.625mm slices as an acceptable compromise between image quality and scanning time.
The field of view should be minimized to focus specifically on the temporal bones, typically ranging from 18-20 centimeters. This targeted approach improves spatial resolution by concentrating the detector elements on the anatomical region of interest rather than imaging unnecessary surrounding structures.
Tube current and voltage settings require careful optimization for temporal bone CT interpretation. Most protocols use 120-140 kVp with tube current adjusted based on patient size, typically ranging from 200-400 mAs. Higher kVp settings help penetrate the dense temporal bone while maintaining adequate soft tissue contrast for middle ear anatomy HRCT evaluation.
Matrix size directly impacts spatial resolution, with 512×512 or higher matrices recommended for temporal bone radiology. The reconstruction interval should match or be smaller than the slice thickness to prevent gaps in anatomical coverage, especially important when creating multiplanar reconstructions.
Patient positioning plays a vital role in image quality. The head should be positioned to align the hard palate parallel to the scanning table, with the temporal bones positioned symmetrically within the gantry. Motion artifacts can severely compromise image quality, so patient cooperation and proper immobilization are essential for successful temporal bone pathology HRCT studies.
Reconstruction algorithms specifically designed for bone imaging enhance the visibility of osseous structures while maintaining adequate soft tissue detail for comprehensive evaluation of both bony and soft tissue components of the temporal bone complex.
External and Middle Ear Anatomical Structures on HRCT
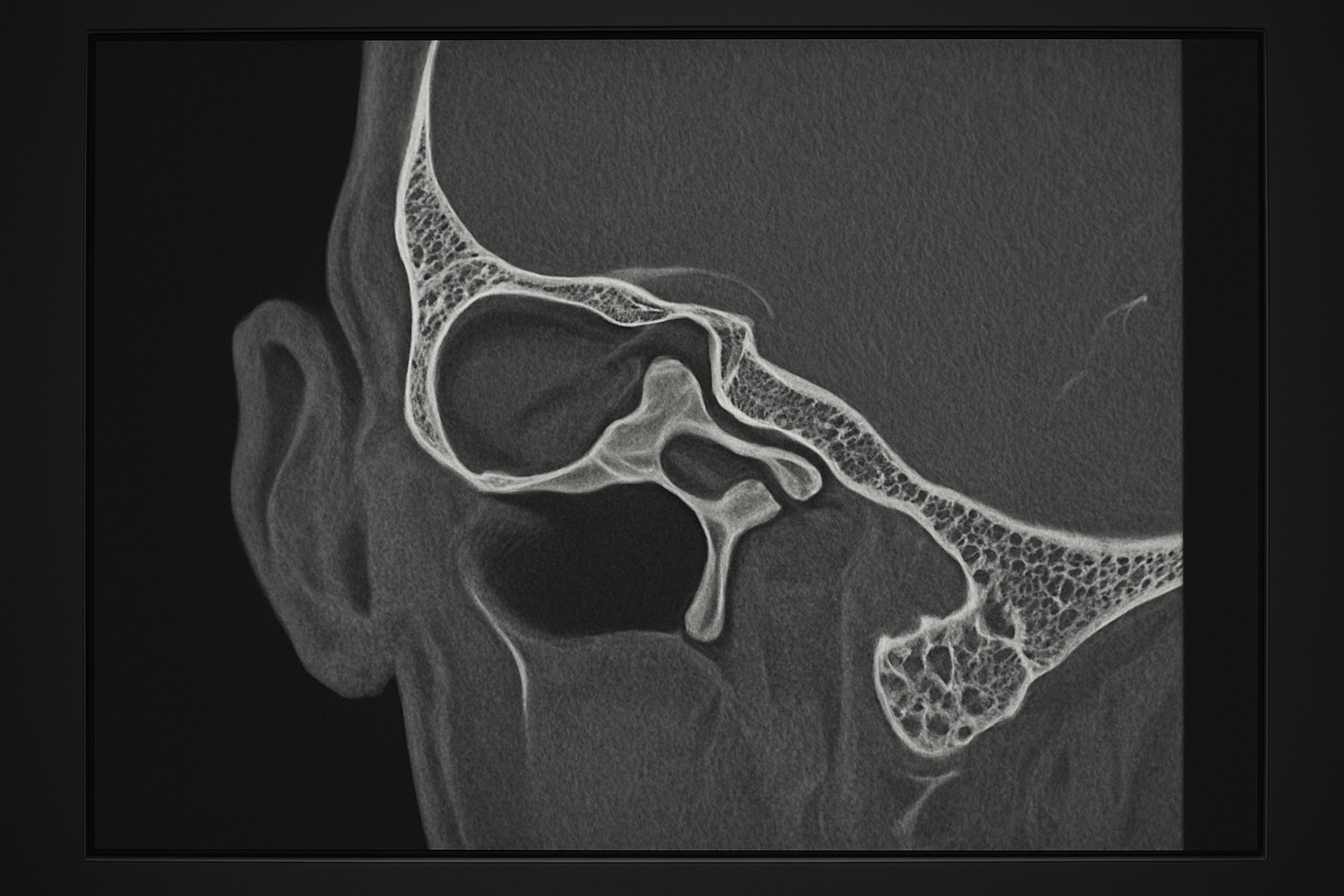
External auditory canal normal appearance and common variants
The external auditory canal (EAC) appears as a distinctive S-shaped air-filled tube on HRCT temporal bone imaging, extending from the auricle to the tympanic membrane. The canal measures approximately 24mm in length and demonstrates two distinct portions: the outer cartilaginous third and the inner bony two-thirds. On axial HRCT images, the EAC shows a characteristic sigmoid configuration with an initial lateral and anterior direction, followed by a medial and slightly posterior course.
Normal canal walls appear smooth and uniform on high resolution CT temporal bone anatomy studies. The anterior and inferior walls are typically thicker than the posterior and superior walls, which can appear quite thin, especially near the temporomandibular joint. The canal diameter varies throughout its length, with the narrowest point usually occurring at the junction between the cartilaginous and bony portions, known as the isthmus.
Common anatomical variants include developmental narrowing of the canal, which can range from mild stenosis to complete atresia. Canal exostoses appear as bilateral, symmetric bony protrusions from the canal walls, most commonly affecting the posterior and anterior walls. These benign growths show characteristic smooth, rounded contours on HRCT imaging and are frequently seen in individuals with chronic cold water exposure.
Another significant variant involves the relationship between the EAC and adjacent structures. The canal may show variable proximity to the temporomandibular joint anteriorly, with some cases demonstrating dehiscent bone between these structures. The posterior canal wall thickness varies considerably, and thin posterior walls can create diagnostic challenges when evaluating for potential complications from middle ear disease.
Tympanic membrane and middle ear cavity identification
The tympanic membrane represents the junction between the external and middle ear spaces on temporal bone imaging. While the membrane itself is rarely visible on HRCT due to its thinness, its position can be inferred from the transition between the air-filled external canal and the middle ear cavity. The membrane typically angles at approximately 45 degrees to the canal axis, with the superior portion positioned more laterally than the inferior portion.
The middle ear cavity, or tympanic cavity, appears as a complex air-filled space bounded by the tympanic membrane laterally and the medial wall of the middle ear. On axial HRCT images, the cavity demonstrates an hourglass configuration, with the mesotympanum representing the central portion at the level of the tympanic membrane. The cavity extends superiorly into the epitympanum (attic) and inferiorly into the hypotympanum.
HRCT ear anatomy clearly demonstrates the ossicular chain within the middle ear space. The malleus head appears in the epitympanum, connected to the incus body through the incudomalleolar joint. The long process of the incus extends inferiorly to articulate with the stapes head through the incudostapedial joint. The stapes footplate sits within the oval window, creating the connection between the middle and inner ear spaces.
The middle ear cavity connects to the mastoid air cells through the aditus ad antrum, a small opening visible in the posterior epitympanum. This connection is important for understanding the spread of inflammatory processes. The Eustachian tube opening appears as a small soft tissue density in the anterior wall of the protympanum on CT temporal bone interpretation studies, representing the cartilaginous portion of this important pressure-equalizing structure.
Inner Ear Complex Anatomy Recognition
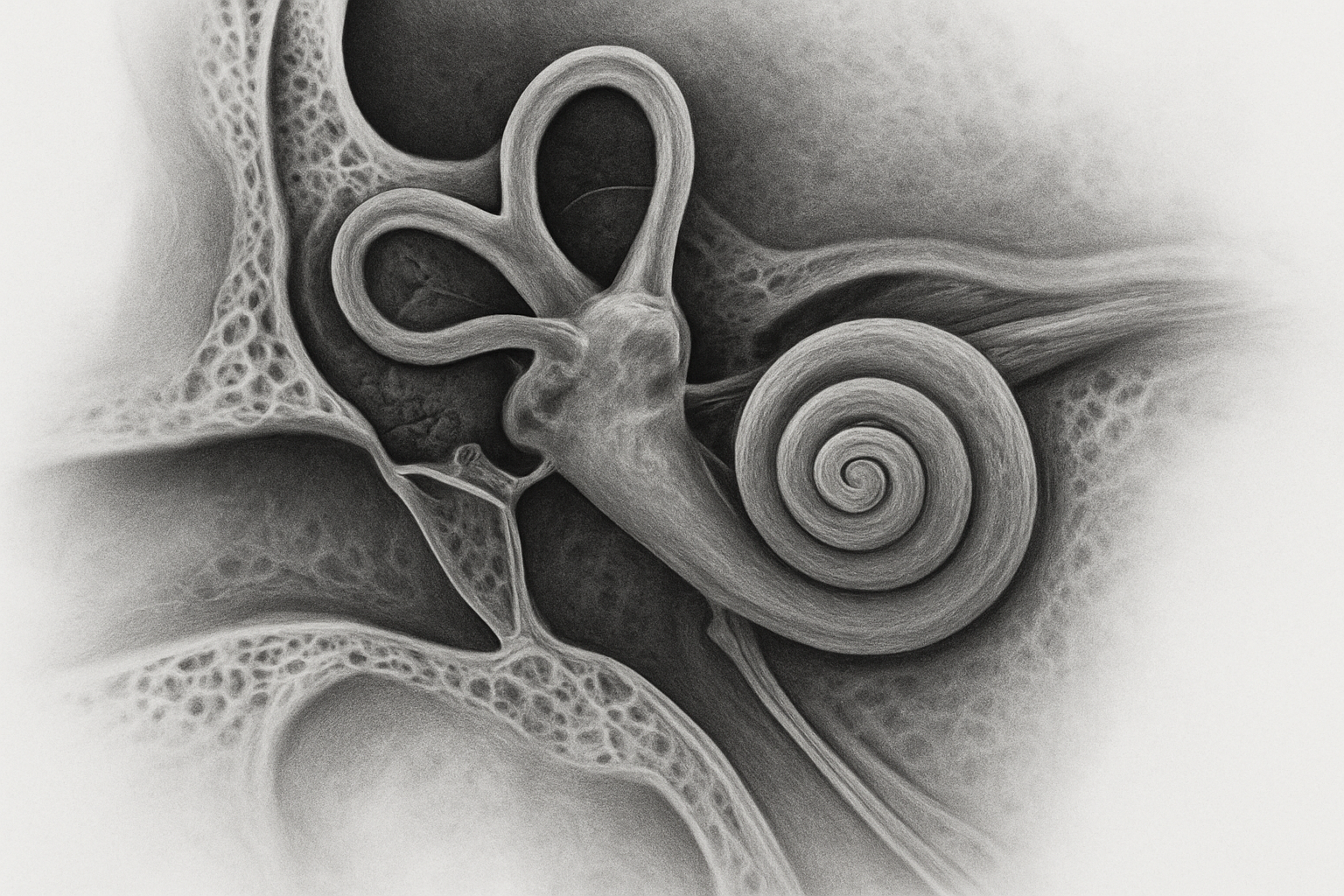
Cochlea Spiral Structure and Internal Acoustic Meatus
The cochlea represents
Pathological Findings and Diagnostic Applications

Inflammatory conditions affecting temporal bone structures
HRCT temporal bone imaging excels at detecting inflammatory processes that affect the complex anatomy of the ear. Chronic otitis media appears as soft tissue opacification within the middle ear cavity, often accompanied by bone erosion of the ossicular chain. The scutum, a thin bony projection that normally protects the incus and malleus, frequently shows erosive changes when chronic infection persists. These erosive patterns help radiologists distinguish between simple fluid accumulation and active inflammatory disease.
Cholesteatoma represents one of the most critical inflammatory conditions visible on high resolution CT temporal bone studies. This acquired condition creates characteristic soft tissue masses that expand and erode surrounding bone structures. The imaging shows non-dependent soft tissue density within the epitympanum or mastoid air cells, with associated bone destruction of the ossicles, tegmen tympani, or facial nerve canal. Early detection through HRCT ear anatomy visualization prevents serious complications like facial nerve paralysis or intracranial extension.
Mastoiditis demonstrates as fluid or soft tissue opacity filling the normally air-filled mastoid air cells. Acute mastoiditis shows widespread opacification with possible bone destruction of the mastoid septa. Chronic mastoiditis creates sclerotic changes where the bone becomes thickened and the air cell system appears obliterated on temporal bone imaging studies.
Labyrinthitis and inflammatory inner ear conditions present as abnormal enhancement patterns or fluid signal within the cochlea, vestibule, or semicircular canals. HRCT temporal bone interpretation helps identify associated bone changes and complications that may require surgical intervention.
Congenital anomalies detection and classification
Temporal bone diagnostic imaging plays a crucial role in identifying congenital malformations that affect hearing and balance function. Microtia and canal atresia represent common outer ear anomalies where the external auditory canal fails to develop properly. HRCT reveals the degree of canal stenosis or complete atresia, along with associated middle ear malformations that impact surgical planning for hearing reconstruction.
Ossicular chain anomalies frequently accompany canal atresia and include malformed or absent malleus, incus, or stapes bones. The imaging clearly demonstrates abnormal ossicular morphology, fusion between bones, or complete absence of ossicular elements. These findings directly influence the surgical approach for hearing restoration procedures.
Inner ear malformations encompass a spectrum of developmental abnormalities affecting the cochlea, vestibule, and semicircular canals. Mondini dysplasia shows characteristic incomplete cochlear development with fewer turns than normal. Large vestibular aqueduct syndrome appears as enlargement of this normally small bony channel, often associated with progressive hearing loss. Semicircular canal dysplasia ranges from mild hypoplasia to complete absence of one or more canals.
Facial nerve canal anomalies include dehiscence where the bone covering the nerve is absent, or aberrant course where the nerve follows an unusual path through the temporal bone. CT temporal bone interpretation identifies these variants that increase surgical risk during middle ear procedures.
Temporal bone pathology HRCT also detects less common conditions like enlarged cochlear aqueduct, common cavity malformation where the cochlea and vestibule form a single space, and labyrinthine aplasia where inner ear structures fail to develop entirely.
Clinical Interpretation Guidelines for Healthcare Professionals
Systematic approach to HRCT temporal bone reading
Developing a structured reading pattern for HRCT temporal bone studies makes the difference between catching subtle pathology and missing critical findings. Start with the external auditory canal and work your way inward through each anatomical compartment systematically.
Begin by checking bone windows at appropriate settings – typically around 4000 HU window width and 700 HU window level. Examine the external auditory canal for stenosis, masses, or bony exostoses that could affect hearing. The tympanic membrane position and middle ear aeration come next, looking for fluid levels, soft tissue masses, or ossicular chain discontinuity.
Pay special attention to the ossicles themselves. The malleus handle should be clearly visible against the tympanic membrane, while the incus body and short process create recognizable landmarks. Ossicular erosion often starts at the incus long process, making this area particularly important during HRCT temporal bone interpretation.
Move systematically to the inner ear structures, checking the cochlea for normal 2.5 turns and intact modiolus. The vestibular system requires careful examination of the semicircular canals for dehiscence or abnormal bone density. The internal auditory canal width should measure less than 8mm, and facial nerve canals need assessment for dehiscence or narrowing.
Don’t forget to evaluate the mastoid air cells for opacification patterns, cholesteatoma, or chronic inflammatory changes. Temporal bone imaging becomes more reliable when you follow the same sequence every time, reducing the chance of overlooking important findings.
Normal variants versus pathological changes differentiation
Distinguishing normal anatomical variations from true pathology represents one of the most challenging aspects of temporal bone radiology. Understanding common variants prevents unnecessary worry and inappropriate treatment recommendations.
High jugular bulb occurs in approximately 6% of patients and can mimic middle ear masses on otoscopy. On HRCT ear anatomy evaluation, the jugular bulb appears as a smooth, rounded soft tissue density that maintains continuity with the jugular vein. True pathological masses typically show irregular borders or enhance differently on contrast studies.
Dehiscent facial nerve canals affect about 25% of patients and usually don’t cause symptoms. The key difference from pathological dehiscence lies in the smooth, well-corticated bone edges seen in developmental variants. Pathological dehiscence from infection or cholesteatoma shows irregular, eroded bone margins with associated soft tissue changes.
Cochlear nerve canal variants include enlarged or duplicated canals that can measure up to 3mm in diameter. These developmental variants maintain smooth, well-defined borders unlike the irregular enlargement seen with acoustic neuromas or other pathological processes.
Mastoid pneumatization patterns vary dramatically between individuals. Poorly pneumatized mastoids with dense bone can look concerning but represent normal variants when symmetric and without associated soft tissue changes. Asymmetric opacification or fluid levels suggest pathological processes requiring further investigation.
The superior semicircular canal dehiscence syndrome requires careful differentiation from normal thin bone over the canal. True dehiscence shows complete absence of bone coverage, while thin bone coverage still maintains some osseous material over the canal on high resolution CT temporal bone anatomy studies.

HRCT scans give us an incredible window into the complex world of temporal bone anatomy. From the tiny structures of the external ear canal to the intricate labyrinth of the inner ear, this imaging technology helps doctors spot everything from chronic infections to congenital abnormalities with remarkable clarity. The ability to see ossicles, cochlear turns, and semicircular canals in such detail has revolutionized how we diagnose and treat ear-related conditions.
For healthcare professionals working with these scans, mastering the normal anatomical landmarks is just the beginning. Recognizing subtle changes that signal disease, understanding when findings are clinically significant, and knowing how to communicate results effectively to patients and colleagues makes all the difference in patient care. Take time to practice identifying these structures regularly, and don’t hesitate to collaborate with radiologists when interpreting challenging cases – your patients will benefit from this careful, thorough approach to temporal bone imaging.