“MRI Brain With DBS Protocol: Safe and Accurate Imaging for Patients With DBS Implants”
MRI Brain With DBS Protocol: Safe Neuroimaging for Deep Brain Stimulation Patients
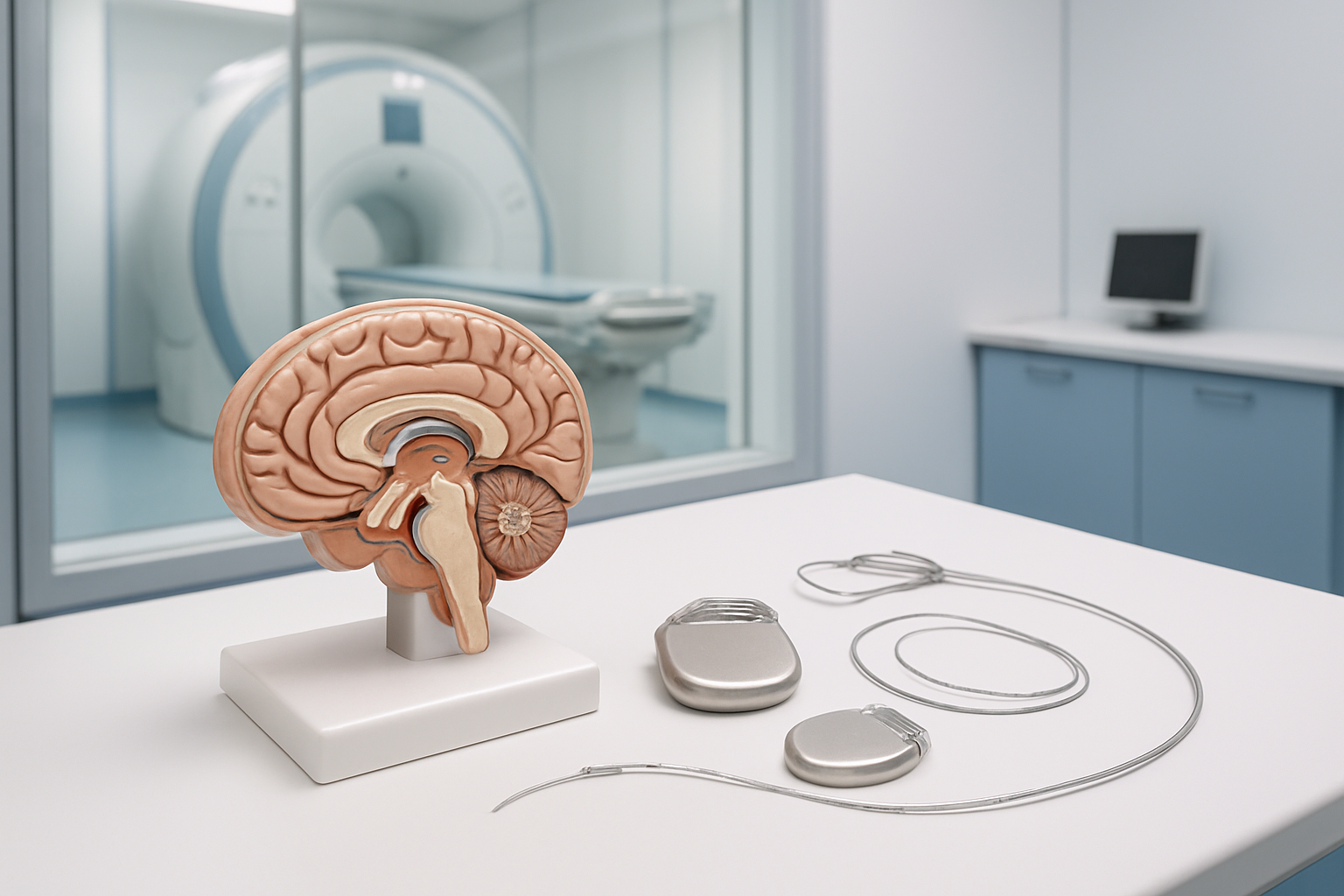
Getting an MRI scan when you have a deep brain stimulation device doesn’t have to be complicated or scary. This comprehensive guide on MRI brain DBS protocol helps radiologists, neurologists, and MRI technologists understand how to safely perform brain imaging on DBS patients while maintaining excellent image quality.
Deep brain stimulation devices require special considerations during MRI scanning, but with the right approach, you can get the diagnostic images you need. We’ll walk you through the essential steps of safe MRI scanning DBS procedures, from checking DBS device MRI compatibility to setting up proper MRI sequence parameters.
You’ll learn how to conduct thorough pre-scan safety assessments that protect your patients, discover the specific imaging techniques that work best for brain MRI with implants, and understand how these protocols benefit clinical diagnosis. Whether you’re new to neuroimaging deep brain stimulation patients or looking to refine your current MRI protocol implanted devices procedures, this guide covers everything you need for confident, safe scanning.
Understanding Deep Brain Stimulation Device Compatibility
MRI Safety Classifications for DBS Systems
Modern DBS devices fall into three distinct MRI safety categories that directly impact scanning protocols and patient care. MR Safe devices contain no magnetic materials and pose no known hazards in any MRI environment, though these are extremely rare in DBS technology. MR Conditional devices represent the majority of contemporary DBS systems, requiring specific scanning conditions to ensure patient safety during MRI brain DBS protocol procedures.
The most critical category involves MR Unsafe or non-conditional devices, which create significant safety risks in magnetic fields. These older DBS systems can experience heating, movement, or malfunction when exposed to MRI environments. The magnetic field strength, specific absorption rate (SAR), and radiofrequency exposure all play crucial roles in determining safe scanning parameters for each device type.
Understanding these classifications becomes essential when developing MRI imaging protocols for DBS patients. Each manufacturer provides detailed technical specifications outlining maximum field strengths, allowable SAR levels, and required sequence modifications. Boston Scientific, Medtronic, and Abbott each maintain different safety thresholds and conditional scanning requirements.
The transition from non-conditional to conditional DBS devices has revolutionized neuroimaging capabilities. Newer systems incorporate improved lead designs, modified pulse generators, and enhanced shielding that allows for diagnostic quality brain imaging while maintaining deep brain stimulation MRI safety standards.
Conditional vs Non-Conditional DBS Devices
Conditional DBS devices represent a major advancement in neuroimaging accessibility for patients with movement disorders. These systems undergo rigorous testing to establish safe MRI scanning parameters, including maximum static magnetic field exposure, gradient switching rates, and radiofrequency power limits. Most conditional devices allow scanning at 1.5T field strengths with specific sequence restrictions and require temporary stimulation suspension during imaging.
Non-conditional DBS systems present significant challenges for MRI brain imaging protocols. These older devices lack the safety testing and design modifications necessary for MRI compatibility. The risks include electrode heating, device malfunction, tissue damage, and potential stimulation parameter changes. Many non-conditional systems require complete explantation before MRI scanning, creating treatment gaps for patients requiring ongoing stimulation therapy.
The key differences extend beyond basic safety classifications. Conditional devices often feature modified electrode designs with reduced heating potential, improved lead materials, and enhanced connector systems. Programming restrictions typically apply, requiring specific stimulation parameters during scanning and careful post-scan assessment of device function.
Patient selection becomes critical when working with mixed device populations. DBS device MRI compatibility directly influences diagnostic capabilities, treatment monitoring, and long-term care planning. Conditional devices enable routine brain imaging for stroke evaluation, tumor surveillance, and surgical planning, while non-conditional systems severely limit these diagnostic options.
Safe MRI scanning DBS protocols must account for device age, manufacturer specifications, and individual patient factors. The evolution from non-conditional to conditional systems continues improving patient care and expanding neuroimaging possibilities for the growing population of DBS patients requiring comprehensive brain imaging.
Pre-Scan Safety Assessment and Patient Preparation

Device Identification and Documentation Review
Before any MRI brain DBS protocol begins, thorough documentation review stands as the cornerstone of patient safety. Medical teams must meticulously verify the exact make, model, and serial number of the implanted deep brain stimulation device. This information directly impacts MRI compatibility decisions and scanning parameters.
The device identification process involves examining the patient’s implant card, surgical records, and manufacturer documentation. Each DBS system carries specific MRI safety ratings – some devices are MR Conditional under certain circumstances, while others may be MR Unsafe. Medtronic, Abbott, and Boston Scientific devices each have distinct MRI guidelines that must be followed precisely.
Documentation should include the implantation date, lead placement locations, and any previous MRI examinations. The time elapsed since implantation affects safety protocols, as newly implanted leads require different handling than well-established systems. Medical staff must also verify the integrity of all system components, including the pulse generator, extension cables, and electrodes.
Patient medical history review extends beyond the DBS device itself. Any additional implanted hardware, such as cardiac pacemakers, cochlear implants, or orthopedic hardware, creates additional complexity for MRI brain DBS protocol planning. Each element requires individual safety assessment to prevent dangerous interactions during scanning.
Programming Device Settings for MRI Compatibility
Programming the DBS device for MRI compatibility represents a critical safety step that directly affects both patient wellbeing and image quality. Most modern DBS systems require specific programming changes before entering the MRI environment to prevent tissue heating and device malfunction.
The standard protocol involves switching the device to MRI mode or completely turning off stimulation, depending on manufacturer specifications. This process typically occurs 30-60 minutes before scanning to allow patients to adjust to temporary stimulation changes. Some patients may experience symptom recurrence during this period, requiring careful monitoring and potential medication adjustments.
Lead impedance testing becomes mandatory before MRI exposure. Abnormal impedance values may indicate lead fracture or insulation breach, conditions that significantly increase MRI risks. Values outside manufacturer-specified ranges typically contraindicate MRI scanning until surgical evaluation occurs.
Battery status verification ensures adequate power reserves for post-scan device reprogramming. Low battery conditions may complicate the return to therapeutic settings following MRI completion. Programming teams must document all parameter changes, including stimulation amplitude, frequency, pulse width, and active electrode configurations.
Post-scan device restoration requires systematic verification of all therapeutic parameters. Staff must confirm proper device function, symptom control restoration, and absence of any stimulation-related complications before patient discharge from the MRI facility.
Optimized MRI Sequence Parameters for DBS Patients

SAR Limitations and Power Restrictions
Specific Absorption Rate (SAR) management becomes critical when scanning DBS patients. The MRI brain DBS protocol requires strict SAR monitoring because metallic components in the stimulator system can create localized heating during radiofrequency transmission. Most DBS manufacturers recommend keeping whole-body SAR below 2.0 W/kg and head SAR below 3.2 W/kg, though specific limits vary by device model and lead configuration.
Temperature rises around DBS electrodes can reach dangerous levels within minutes at standard SAR levels. The heating primarily occurs at electrode-tissue interfaces where current density concentrates. MRI sequence parameters must be adjusted to maintain SAR levels well below manufacturer thresholds, typically requiring 50% reduction from normal scanning protocols.
Power restrictions directly impact sequence selection and timing parameters. High SAR sequences like fast spin echo and gradient echo with short repetition times need modification or replacement with lower power alternatives. Turbo STIR sequences, commonly used for brain imaging, often exceed safe SAR limits for DBS patients and require alternative approaches.
Real-time SAR monitoring becomes essential during scanning sessions. Modern MRI systems calculate SAR continuously, but technologists must verify calculations match DBS device specifications. Some facilities use external SAR monitoring equipment for additional safety verification when imaging deep brain stimulation patients.
Gradient Field Considerations and Slew Rate Adjustments
Gradient switching during MRI scanning creates time-varying magnetic fields that can induce currents in DBS leads, potentially affecting device function or causing unwanted stimulation. Safe MRI scanning DBS protocols require careful attention to gradient slew rates and maximum gradient amplitudes to prevent these interactions.
Standard gradient slew rates often exceed manufacturer recommendations for DBS device MRI compatibility. Most DBS systems require slew rate reductions to 20-30 T/m/s compared to normal rates of 100-200 T/m/s. This reduction significantly impacts sequence timing and image acquisition speed, requiring protocol modifications throughout the imaging session.
Maximum gradient strength limitations also affect sequence selection. While 3T scanners typically operate at gradients up to 40-80 mT/m, DBS protocols often restrict gradients to 10-20 mT/m. These restrictions particularly impact diffusion-weighted imaging and functional MRI sequences that rely on strong gradient performance for optimal results.
Echo planar imaging sequences face the greatest challenges under gradient restrictions. The rapid gradient switching essential for EPI acquisition often violates DBS safety parameters. Alternative approaches include reducing matrix size, increasing echo spacing, or switching to spin echo sequences with longer acquisition times but better safety profiles.
Gradient duty cycle management prevents sustained high-amplitude switching that could affect DBS device operation. Interleaving sequences with gradient-free periods allows adequate cooling time and reduces cumulative effects on the implanted system. This approach maintains image quality while respecting neuroimaging deep brain stimulation safety requirements.
Image Quality Enhancement Techniques

Artifact Reduction Strategies Around Hardware
Metal artifacts from DBS electrodes and pulse generators create significant challenges in brain MRI imaging. The key to minimizing these artifacts lies in smart positioning and parameter adjustments that work around the hardware rather than against it.
Patient positioning plays a crucial role in artifact management. Orienting the DBS leads parallel to the main magnetic field (B0) dramatically reduces susceptibility artifacts. This means positioning patients with their head aligned so the electrode trajectories run along the scanner’s z-axis. When this isn’t possible, slight head tilting can help minimize the worst artifacts around critical brain regions.
Bandwidth optimization serves as another powerful tool. Increasing the receiver bandwidth reduces chemical shift artifacts and minimizes distortion around metallic components. While this approach may slightly decrease signal-to-noise ratio, the trade-off usually favors improved image quality around DBS hardware.
Phase and frequency encoding direction selection significantly impacts artifact appearance. Switching phase encoding to minimize artifacts over regions of interest often provides better visualization of target brain structures. The artifacts get redistributed rather than eliminated, but strategic placement keeps them away from diagnostically important areas.
Shimming adjustments become even more critical with DBS patients. Advanced shimming techniques help compensate for magnetic field inhomogeneities created by the metallic implants. Many modern scanners offer specialized shimming protocols designed specifically for patients with implanted devices, automatically adjusting field homogeneity around known artifact-producing areas.
Specialized Pulse Sequences for Metal Implants
Modern MRI sequences have evolved specifically to address challenges posed by metallic implants like DBS systems. These specialized techniques work by manipulating radiofrequency pulses and gradient timing to reduce metal-induced artifacts while maintaining diagnostic image quality.
MARS (Metal Artifact Reduction Sequence) represents a significant advancement in DBS patient imaging. This technique uses view-angle tilting combined with high-bandwidth imaging to minimize distortion around metallic objects. MARS works particularly well for visualizing brain tissue adjacent to DBS electrodes, providing clearer anatomical detail than conventional sequences.
SEMAC (Slice Encoding for Metal Artifact Correction) offers another powerful approach for DBS MRI protocols. This method corrects for through-plane distortions by encoding additional spatial information, effectively “unwrapping” the distorted tissue around metal implants. SEMAC proves especially valuable when assessing electrode placement accuracy or evaluating surrounding brain structures.
WARP (Wide-band Application with Relaxed Pulses) sequences provide excellent soft tissue contrast while minimizing artifacts from DBS hardware. These sequences use specially designed radiofrequency pulses that maintain image quality even in the presence of significant magnetic field disturbances caused by metallic components.
Fast spin-echo sequences with short echo trains work well for routine brain imaging in DBS patients. These sequences reduce sensitivity to magnetic susceptibility effects while providing good anatomical detail. T2-weighted images using these parameters often show less artifact interference around electrode sites compared to gradient-echo sequences.
Clinical Applications and Diagnostic Benefits

Post-Surgical Lead Placement Verification
MRI brain DBS protocol plays a vital role in confirming accurate electrode placement following deep brain stimulation surgery. Surgeons rely on high-resolution imaging to verify that DBS leads are positioned correctly within target brain structures like the subthalamic nucleus or globus pallidus. The precision required for optimal therapeutic outcomes makes post-operative verification absolutely essential.
Safe MRI scanning DBS protocols enable detailed visualization of lead trajectories and tip locations without compromising patient safety. Modern DBS device MRI compatibility allows radiologists to obtain clear images that show electrode positioning relative to anatomical landmarks. This verification process helps identify any potential placement errors that could affect treatment efficacy or cause unwanted side effects.
The imaging protocol must balance image quality with safety considerations. MRI sequence parameters are carefully adjusted to minimize heating around the implanted hardware while maintaining sufficient resolution for accurate assessment. T2-weighted sequences typically provide excellent contrast for visualizing brain structures and electrode positions, while susceptibility-weighted imaging can help detect any bleeding or tissue changes around the leads.
Documentation of lead placement serves both immediate clinical needs and long-term patient management. These baseline images become reference points for future comparisons and help neurologists optimize stimulation parameters. When patients experience suboptimal responses or new symptoms, comparing current imaging to post-surgical verification scans can reveal lead migration or other hardware-related issues that might require intervention.
Long-Term Device Monitoring and Complications
MRI imaging DBS patients over time provides invaluable insights into device integrity and potential complications that may develop months or years after implantation. Regular monitoring through neuroimaging deep brain stimulation protocols helps detect hardware failures, lead fractures, or tissue reactions before they become clinically significant problems.
Battery depletion represents one of the most common long-term issues requiring MRI evaluation. As implantable pulse generators reach end-of-life, MRI protocol implanted devices can help assess any changes in lead positioning or surrounding tissue that might complicate battery replacement procedures. This proactive approach helps surgeons plan replacement strategies and anticipate potential challenges.
Lead migration, though relatively uncommon, can significantly impact therapeutic outcomes. DBS patient MRI preparation for follow-up imaging allows detection of subtle positional changes that might explain declining symptom control or emerging side effects. Early identification of migration enables timely intervention before patients experience significant symptom recurrence.
Infection remains a serious complication requiring prompt recognition and treatment. MRI can reveal inflammatory changes around hardware components, helping differentiate infection from normal post-surgical healing. Brain MRI with implants protocols are specifically designed to highlight tissue changes while avoiding artifacts that might obscure important findings.
Tissue reactions, including fibrosis or cystic changes around electrodes, can develop over time and affect stimulation efficiency. Regular imaging surveillance helps neurologists understand why some patients may require programming adjustments or experience gradual symptom return despite stable hardware function.
Getting MRI scans for patients with Deep Brain Stimulation devices doesn’t have to be complicated when you follow the right protocols. The key is making sure the DBS system is compatible with MRI scanning, preparing patients properly with safety checks, and using the right imaging sequences that work well with the device. When radiologists apply specific enhancement techniques, they can get clear, diagnostic-quality images that help doctors make better treatment decisions for their patients.
The real game-changer comes from understanding how DBS devices interact with MRI technology and adjusting your approach accordingly. By sticking to proven safety protocols and optimized scanning parameters, medical teams can confidently provide comprehensive neurological evaluations for DBS patients. This opens up better monitoring of treatment progress and more accurate diagnosis of any new neurological issues that might come up. If you’re working with DBS patients, take the time to master these specialized protocols – your patients will benefit from the improved care and diagnostic capabilities.