“From neck pain to nerve compression—MRI C V Junction helps doctors find the root cause with precision.”
MRI Cervico-Vertebral Junction: A Complete Guide to CV Junction Imaging
The MRI cervico-vertebral junction represents one of the most complex anatomical regions to evaluate, where your skull meets your upper cervical spine. This critical area houses vital structures that can impact everything from basic movement to neurological function.
This comprehensive guide is designed for radiologists, neurologists, orthopedic surgeons, and medical residents who need to master CV junction anatomy MRI interpretation and recognize key pathological findings.
We’ll walk you through essential MRI sequences that provide the clearest views of the atlantooccipital joint MRI and surrounding structures, helping you choose the right imaging protocols for different clinical scenarios. You’ll also learn to identify common pathological conditions including basilar invagination MRI findings, Chiari malformation imaging characteristics, and other craniocervical junction pathology that frequently appears in this region.
Finally, we’ll cover the critical measurements and assessment parameters that separate normal variants from clinically significant abnormalities, giving you the confidence to provide accurate diagnoses when cervical spine MRI upper studies cross your desk.
Understanding MRI Cervico-Vertebral Junction Anatomy
Key Anatomical Structures Visualized on MRI
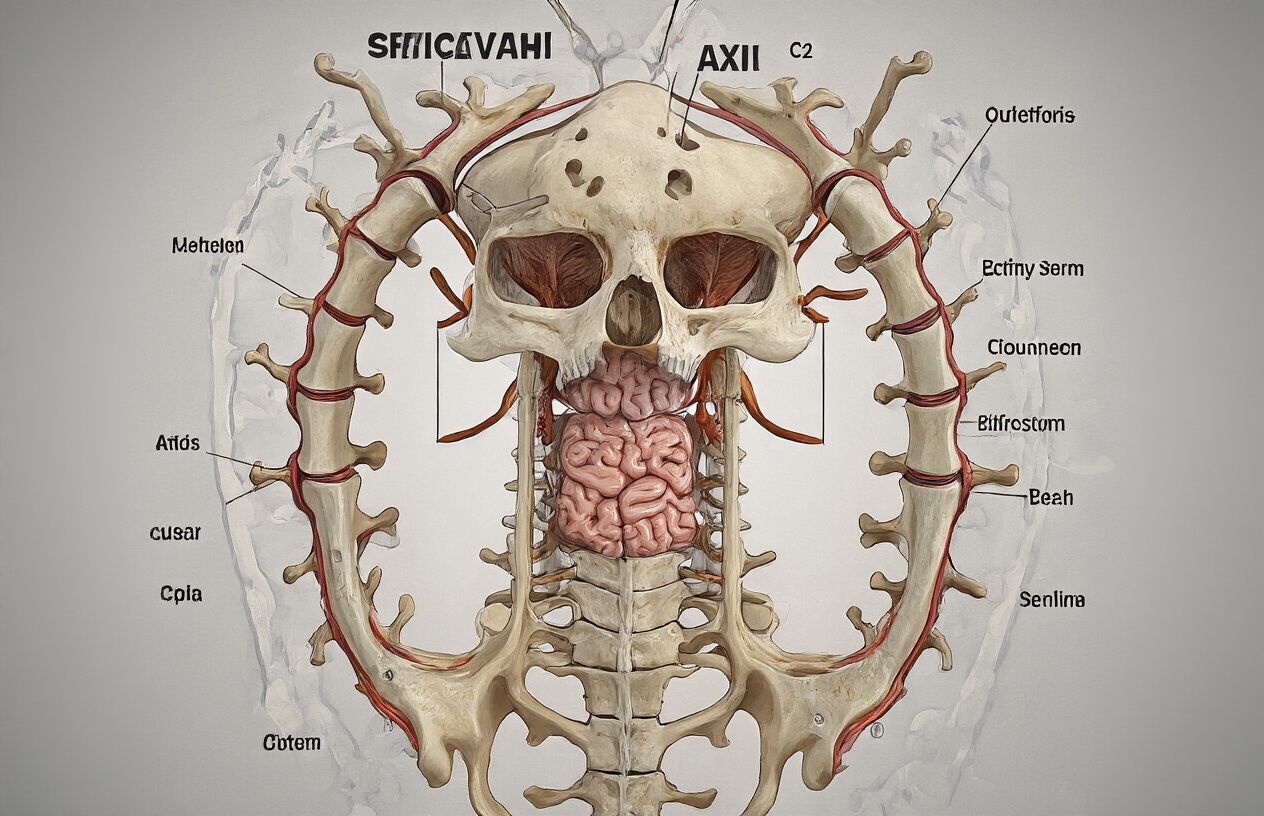
The MRI cervico-vertebral junction provides exceptional visualization of complex anatomical structures that form the critical transition zone between the skull and cervical spine. The foramen magnum serves as the central opening where the medulla oblongata transitions into the spinal cord, creating the cervicomedullary junction that’s clearly visible on sagittal T2-weighted sequences.
The atlas (C1) and axis (C2) vertebrae demonstrate unique morphology on CV junction anatomy MRI. The atlas lacks a vertebral body and consists of anterior and posterior arches connected by lateral masses. The atlantooccipital joint MRI reveals the articulation between the occipital condyles and superior facets of C1, while the atlantoaxial joint shows the relationship between C1 and the odontoid process of C2.
The odontoid process (dens) appears as a tooth-like projection extending superiorly from the C2 vertebral body. This structure maintains crucial alignment relationships with the anterior arch of C1 and the basion of the skull. The transverse ligament of the atlas, visible on axial images, prevents excessive anterior translation of C1 on C2.
Vascular structures include the vertebral arteries as they course through the foramen transversarium of C1 and C2, then penetrate the atlantooccipital membrane. The posterior inferior cerebellar arteries (PICA) and anterior spinal arteries are often identifiable on high-resolution sequences.
The craniocervical junction pathology becomes apparent when examining the tectorial membrane, alar ligaments, and joint capsules. These soft tissue structures provide stability and are best visualized using proton density or T2-weighted sequences with fat suppression.
Normal Anatomical Relationships and Measurements
Craniovertebral junction imaging relies on specific measurements to assess normal anatomical relationships and identify pathological conditions. The atlantooccipital joint MRI demonstrates normal positioning when the basion-dental interval measures less than 12mm in adults and less than 5mm in children.
The atlantodental interval (ADI) represents the distance between the posterior aspect of the anterior arch of C1 and the anterior surface of the odontoid process. Normal values should not exceed 3mm in adults and 4-5mm in children on flexion views. This measurement helps identify atlantoaxial instability and ligamentous injury.
Basilar invagination MRI assessment uses Chamberlain’s line, drawn from the posterior hard palate to the posterior margin of the foramen magnum. The odontoid tip should lie below this line by at least 3mm. McGregor’s line extends from the posterior hard palate to the most caudal point of the occipital curve, with the odontoid tip normally positioned 4.5mm below this reference.
The cervicomedullary junction imaging shows the normal cervical lordosis beginning at the atlantooccipital joint. The clivus-canal angle, measured between the clivus and posterior wall of the spinal canal, typically ranges from 150-180 degrees. Values outside this range may suggest craniovertebral anomalies.
Chiari malformation imaging requires assessment of cerebellar tonsillar position relative to the foramen magnum. Normal tonsils should not extend more than 5mm below the McRae line (drawn from the basion to the opisthion). The fourth ventricle maintains its normal diamond shape and position above the foramen magnum in healthy individuals.
The posterior atlantooccipital membrane distance from the occiput measures approximately 4-6mm, while the atlantoaxial joint space maintains uniform width of 2-3mm. These cervical spine MRI upper measurements help distinguish normal variants from pathological conditions requiring intervention.
Essential MRI Sequences for CV Junction Imaging

T1-weighted imaging benefits and applications
T1-weighted sequences serve as the cornerstone for evaluating MRI cervico-vertebral junction anatomy, providing exceptional detail of bone structures and craniovertebral junction imaging. These sequences excel at demonstrating the osseous architecture of the atlantooccipital joint MRI, clearly delineating cortical bone margins and identifying areas of bone marrow edema or pathological enhancement.
The superior soft tissue contrast in T1-weighted imaging makes it invaluable for assessing the cervico-medullary junction imaging, particularly when evaluating for mass lesions or inflammatory processes. Fat-saturated T1 sequences with gadolinium enhancement become essential when investigating suspected infections, tumors, or inflammatory conditions affecting the CV junction anatomy MRI.
Pre-contrast T1 sequences effectively demonstrate anatomical landmarks crucial for CV junction measurements MRI, including the basion, opisthion, and anterior arch of C1. The clear visualization of these structures allows radiologists to perform accurate morphometric assessments and detect subtle abnormalities in craniocervical junction pathology.
Post-contrast T1 imaging proves particularly valuable in cases of suspected basilar invagination MRI or when evaluating for associated syrinx formation. The enhancement patterns help differentiate between various pathological processes and provide critical information about tissue vascularity and blood-brain barrier integrity at this complex anatomical region.
T2-weighted sequences for optimal tissue contrast
T2-weighted sequences provide unparalleled visualization of the neural structures and cerebrospinal fluid spaces around the cervical spine MRI upper region. These sequences excel at demonstrating the relationship between the brainstem, upper cervical cord, and surrounding CSF, making them indispensable for Chiari malformation imaging and related pathologies.
The exceptional contrast between CSF and neural tissue in T2-weighted imaging allows for precise evaluation of CSF flow dynamics and identification of compression at the foramen magnum. This becomes particularly important when assessing patients with suspected cerebellar tonsillar herniation or other causes of cervicomedullary compression.
STIR (Short Tau Inversion Recovery) sequences, a specialized form of T2-weighted imaging, provide excellent fat suppression while maintaining high sensitivity to pathological processes. These sequences prove invaluable for detecting bone marrow edema, ligamentous injuries, and inflammatory changes that might not be apparent on conventional T2 sequences.
T2 sagittal and axial planes work synergistically to provide comprehensive coverage of the craniovertebral junction imaging. Sagittal images demonstrate the overall alignment and relationship of structures, while axial images provide cross-sectional detail of neural compression and bone abnormalities. The combination allows for thorough assessment of both static and dynamic abnormalities affecting this critical transitional zone between the skull and cervical spine.
Common Pathological Conditions Detected

Atlantoaxial Instability and Subluxation Patterns
Atlantoaxial instability represents one of the most clinically significant findings on MRI cervico-vertebral junction studies. This condition involves abnormal movement between the C1 (atlas) and C2 (axis) vertebrae, which can compress the spinal cord and brainstem with potentially devastating consequences.
The normal atlantoaxial relationship maintains strict dimensional parameters. The atlantodental interval (ADI) should measure less than 3mm in adults and less than 4mm in children on flexion views. When craniocervical junction pathology develops, this interval widens significantly, indicating ligamentous failure or bony abnormalities.
MRI excels at demonstrating the soft tissue components involved in atlantoaxial stability. The transverse ligament of the atlas, cruciate ligaments, and alar ligaments appear as low-signal structures on most sequences. When these ligaments tear or stretch, they show increased signal intensity on T2-weighted images, often with associated thickening or discontinuity.
Several subluxation patterns emerge in cervico-medullary junction imaging. Anterior atlantoaxial subluxation occurs when C1 slides forward on C2, typically seen in rheumatoid arthritis or trauma. Posterior subluxation, though less common, can result from odontoid fractures or congenital anomalies. Rotatory subluxation creates a complex three-dimensional deformity that MRI captures beautifully in multiple planes.
Atlantooccipital joint MRI sequences should include high-resolution T1 and T2-weighted sagittal images, along with STIR sequences to detect bone marrow edema. Axial images help evaluate the lateral masses and facet joints, while coronal views assess lateral displacement patterns.
Basilar Invagination and Cranial Settling
Basilar invagination represents a complex craniocervical junction pathology where the odontoid process projects abnormally into the foramen magnum. This condition can be primary (congenital) or secondary (acquired through conditions like rheumatoid arthritis, Paget’s disease, or osteogenesis imperfecta).
Basilar invagination MRI requires precise measurement techniques to establish diagnosis. The Chamberlain line, drawn from the posterior hard palate to the posterior margin of the foramen magnum, serves as a key reference. When the tip of the odontoid extends more than 3mm above this line, basilar invagination is present. The McRae line, connecting the anterior and posterior lips of the foramen magnum, provides another critical measurement – the odontoid tip should not cross this boundary.
Cranial settling differs from basilar invagination in its mechanism. This condition involves the skull literally “settling” down onto the cervical spine, often seen in patients with atlantooccipital assimilation, rheumatoid arthritis, or connective tissue disorders. The result creates similar clinical presentations but requires different therapeutic approaches.
CV junction anatomy MRI demonstrates the relationship between the brainstem and surrounding bony structures with exceptional detail. T2-weighted sagittal sequences clearly show cerebrospinal fluid spaces and can reveal compression of the medulla oblongata or upper cervical cord. When basilar invagination or cranial settling occurs, these images show crowding at the foramen magnum with potential effacement of the cisterna magna.
The clinical implications of these conditions cannot be overstated. Patients may present with headaches, neck pain, dysphagia, respiratory difficulties, or progressive neurological deterioration. Cervical spine MRI upper sequences must capture the entire craniocervical transition to avoid missing these potentially life-threatening abnormalities.
Critical Measurements and Assessment Parameters

Atlanto-dental interval evaluation techniques
The atlanto-dental interval (ADI) represents one of the most critical measurements in MRI cervico-vertebral junction assessment. This measurement evaluates the space between the posterior aspect of the anterior arch of C1 and the anterior surface of the odontoid process of C2. Normal ADI values should not exceed 3mm in adults and 5mm in children on neutral positioning.
When performing ADI measurements on cervical spine MRI upper sequences, radiologists must use sagittal T1 or T2-weighted images that clearly demonstrate both anatomical structures. The measurement should be taken perpendicular to the long axis of the odontoid process at its widest point. Dynamic flexion-extension studies can reveal atlantoaxial instability when the ADI increases beyond normal limits during neck flexion.
Several factors can affect ADI measurements, including patient positioning, image quality, and the presence of degenerative changes. Inflammatory conditions like rheumatoid arthritis commonly cause atlantoaxial subluxation, resulting in increased ADI values. Trauma-related injuries to the transverse ligament can also lead to abnormal widening of this interval.
CV junction measurements MRI protocols should include both neutral and dynamic positioning when atlantoaxial instability is suspected. The radiologist must carefully assess for associated spinal cord compression, which often occurs when the ADI exceeds 8-10mm. T2-weighted sequences are particularly valuable for detecting cord signal changes that may accompany atlantoaxial subluxation.
McRae’s line and foramen magnum relationships
McRae’s line serves as a fundamental reference point in craniovertebral junction imaging, connecting the anterior and posterior margins of the foramen magnum on midsagittal MRI images. This anatomical landmark helps assess basilar invagination MRI findings and other craniocervical junction abnormalities.
The odontoid tip should normally remain below McRae’s line. When the odontoid process extends more than 5mm above this line, basilar invagination is diagnosed. This condition can compress the brainstem and upper cervical spinal cord, leading to serious neurological complications. Chiari malformation imaging often reveals associated tonsillar herniation below the foramen magnum, which can be measured relative to McRae’s line.
Chamberlain’s line represents another important measurement tool, extending from the hard palate to the posterior margin of the foramen magnum. The odontoid tip should not project more than 3mm above Chamberlain’s line in normal individuals. These measurements become particularly relevant when evaluating patients with congenital anomalies, inflammatory arthropathies, or metabolic bone diseases.
Craniocervical junction pathology assessment requires careful evaluation of multiple anatomical relationships. The clivus-canal angle, measured between the clivus and posterior cervical line, normally ranges between 150-180 degrees. Acute angles may indicate cranial settling or basilar invagination.
Cervico-medullary junction imaging must include assessment of the cerebrospinal fluid spaces around the brainstem and upper spinal cord. Crowding at the foramen magnum can compromise CSF flow and lead to syringomyelia formation. Proper measurement techniques ensure accurate diagnosis and appropriate treatment planning for these complex anatomical relationships.
Clinical Symptoms Requiring CV Junction MRI

Neurological deficits indicating upper cervical pathology
Patients presenting with specific neurological symptoms often require MRI cervico-vertebral junction imaging to identify potential upper cervical spine pathology. Myelopathy signs represent the most concerning indication, including progressive weakness in both upper and lower extremities, hyperreflexia, and positive Babinski signs. These symptoms suggest compression of the cervico-medullary junction, which can occur in conditions like basilar invagination or atlantoaxial subluxation.
Gait disturbances frequently accompany upper cervical pathology, manifesting as spastic or ataxic walking patterns. Patients may experience difficulty with fine motor coordination, including problems with handwriting, buttoning clothes, or handling small objects. These deficits arise from disruption of the corticospinal tracts at the craniocervical junction.
Sensory abnormalities provide additional clues for craniovertebral junction imaging. Loss of proprioception and vibration sense in the hands and feet, along with altered temperature sensation, can indicate dorsal column dysfunction. Some patients develop neuropathic pain patterns that radiate from the occiput down the cervical spine.
Cranial nerve involvement may occur when pathology extends rostrally, causing diplopia, dysphagia, or facial numbness. Drop attacks or sudden falls without loss of consciousness can result from vertebrobasilar insufficiency secondary to vascular compression at the CV junction. Sleep apnea occasionally develops when medullary respiratory centers face compression, making cervico-medullary junction imaging critical for proper diagnosis.
Chronic neck pain with mechanical instability signs
Chronic neck pain combined with mechanical instability symptoms warrants comprehensive CV junction anatomy MRI evaluation. Patients typically describe pain that worsens with head movement, particularly during rotation or extension. The pain often has a sharp, shooting quality that may radiate into the occiput or upper shoulders.
Mechanical instability manifests through several characteristic signs. Patients report a sensation of their head feeling “loose” or unstable on their neck, especially when transitioning from lying to sitting positions. Some describe hearing clicking or popping sounds during neck movements, which may indicate abnormal motion between the atlas and axis or at the atlantooccipital joint.
Positional symptoms represent another key indicator for MRI evaluation. Pain that significantly improves when the head is supported, such as when lying down or wearing a cervical collar, suggests mechanical compromise. Conversely, symptoms that worsen with upright positioning or prolonged sitting may indicate inadequate support structures at the craniocervical junction.
Muscle spasm and tension frequently accompany mechanical instability. Patients often develop compensatory muscle guarding in the suboccipital region, leading to persistent headaches and neck stiffness. The pain pattern may follow specific distributions, including C1-C2 dermatomes, helping localize the pathology.
Chiari malformation imaging becomes relevant when patients experience positional headaches that worsen with coughing, sneezing, or Valsalva maneuvers, as these symptoms may indicate associated tonsillar herniation alongside mechanical instability at the CV junction.
Interpretation Guidelines for Radiologists

Systematic approach to image analysis
Begin your MRI cervico-vertebral junction evaluation with a consistent checklist approach. Start by examining the sagittal T2-weighted images to assess overall alignment and identify any obvious abnormalities. Look at the relationship between the skull base and upper cervical vertebrae, paying particular attention to the atlantooccipital joint positioning and the odontoid process alignment.
Move systematically through the craniovertebral junction imaging by evaluating bone morphology first. Check for developmental anomalies like basilar invagination, platybasia, or atlantooccipital assimilation. Measure key parameters including the McRae line, Wackenheim’s line, and the atlanto-dental interval to quantify any abnormal relationships.
Next, assess soft tissue structures. Examine the cervico-medullary junction for signal abnormalities, compression, or displacement. Look carefully at the cerebellar tonsils for signs of Chiari malformation imaging findings, noting their position relative to the foramen magnum. The brainstem should be evaluated for signal changes, mass effect, or distortion.
Review the vertebral arteries in their course through the transverse foramina and around the atlas. Check for adequate flow voids on T2-weighted sequences and look for any compression or displacement. Assess the ligamentous structures, particularly the transverse ligament of the atlas and the alar ligaments when high-resolution sequences are available.
Complete your evaluation by correlating findings across all imaging planes. Axial images help confirm suspicious findings from sagittal views and provide better visualization of lateral structures and potential asymmetries in the CV junction anatomy MRI.
Pitfalls and common misinterpretation errors
Normal anatomical variants often create diagnostic confusion in craniocervical junction pathology interpretation. The most frequent error involves mistaking a prominent occipital condyle or assimilation anomaly for pathological basilar invagination. Always use multiple measurement techniques and reference normal values specific to your patient population.
Cerebrospinal fluid flow artifacts can mimic syrinx formation or cord signal abnormalities on T2-weighted images. These artifacts typically appear as linear hyperintense signals within the spinal cord and can be differentiated by their characteristic appearance on flow-sensitive sequences or by using cardiac-gated imaging protocols.
Positioning artifacts significantly impact CV junction measurements MRI accuracy. Images obtained with the patient’s head in flexion or extension can falsely suggest instability or create apparent compression that doesn’t exist in neutral positioning. Always verify patient positioning and consider repeat imaging if measurements seem inconsistent with clinical findings.
Partial volume effects commonly affect small structures at the craniovertebral junction. The thin cortical bone of the occipital condyles and atlas can appear disrupted on thick-slice sequences, leading to false impressions of fracture or erosion. Use thin-section imaging when evaluating these delicate structures.
Signal intensity variations in the upper cervical cord require careful interpretation. Age-related changes, previous trauma, or technical factors can create signal alterations that mimic pathology. Compare with clinical symptoms and consider the patient’s age and medical history when evaluating subtle signal changes in the cervical spine MRI upper segments.

The cervico-vertebral junction represents one of the most complex anatomical regions that radiologists encounter, demanding specialized knowledge of both normal anatomy and pathological variations. From mastering the essential MRI sequences to understanding critical measurements like the basion-dens interval and Chamberlain’s line, accurate CV junction imaging requires a systematic approach that combines technical expertise with clinical correlation.
When patients present with symptoms ranging from neck pain and headaches to more serious neurological deficits, MRI of the CV junction can reveal crucial pathological conditions including atlantoaxial instability, basilar invagination, and Chiari malformations. For radiologists working with these challenging cases, developing a consistent interpretation framework that incorporates both quantitative measurements and qualitative assessment will improve diagnostic accuracy and patient outcomes. Remember that collaboration with clinicians and understanding the specific clinical questions being asked will always enhance the value of your radiological expertise in this critical anatomical region.


